Factors associated with acute health problems in premature infants
DOI:
https://doi.org/10.35699/reme.v28i1.37985Keywords:
Signs and Symptoms, Infant, Premature, Pediatric Nursing, Longitudinal StudiesAbstract
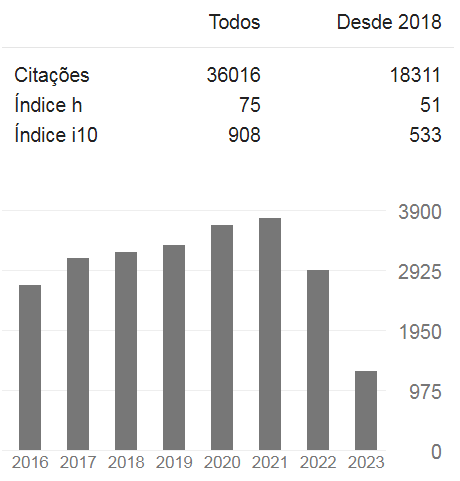
Objective: to analyze neonatal and socioeconomic factors associated with the development of acute health problems in late and moderate preterm infants in the first year of life. Method: longitudinal epidemiological study, in which 151 premature babies (born with a gestational age of 32 to 37 incomplete weeks) were followed during the first year of life. Data collection occurred, quarterly, using a characterization instrument with neonatal and socioeconomic variables. Monitoring took place using forms, applied via telephone call to parents of premature babies, to identify acute health problems. The data were subjected to analytical statistics using Pearson's correlation. Results: acute illnesses showed a linear trend throughout the first year of life. Gastrointestinal disorders were more frequent in the first months, and skin allergies and respiratory disorders occurred more frequently at the end of the first year of life. Neonatal vitality was a factor associated with greater intensity of acute illnesses. Conclusion: the intensity of acute illnesses has a significant correlation with neonatal factors in the first trimester of life.
References
World Health Organization (WHO). Preterm birth. 2018[citado em 2019 ago. 9];363. Disponível em: https://www.who.int/en/news-room/fact-sheets/detail/preterm-birth
Machado MCHS, Santiloni AFP, Ferrari AP, Parada CMGL, Carvalhaes MABL, Tonete VLP. Atenção à saúde no primeiro ano de vida de uma coorte prospectiva de lactentes prematuros tardios e a termo de Botucatu, São Paulo, 2015-2017. Epidemiol. Serv Saúde [Internet]. 2021[citado em 2022 jan. 11];30(2):e2020619. Disponível em: http://dx.doi.org/10.1590/s1679-49742021000200014.
Delnord M, Zeitlin J. Epidemiology of late preterm and early term births – An international perspective. Semin Fetal Neonatal Med [Internet]. 2019[citado em 2022 jan. 4];24(1):3-10. Disponível em: https://doi.org/10.1016/j.siny.2018.09.001
Engle WA. A recommendation for the definition of "late preterm" (near-term) and the birth weight-gestational age classification system. Semin Perinatol [Internet]. 2006[citado em 2022 jan. 4];30(1):2-7. Disponível em: https://doi.org/10.1053/j.semperi.2006.01.007
Ministério da Saúde (BR). Banco de dados do Sistema Único de Saúde - DATASUS. 2018 [citado em 2018 maio 20]. Disponível em: http://www.datasus.gov.br.
Huff K, Rose RS, Engle WA. Late Preterm Infants: Morbidities, Mortality, and Management Recommendations. Pediatr Clin North America [Internet]. 2019[citado em 2022 jan. 5];66(2):387-402. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30819344/
McLaurin KK, Wade SW, Kong AM, Diakun D, Olajide IR, Germano J. Characteristics and health care utilization of otherwise healthy commercially and Medicaid-insured preterm and full-term infants in the US. Pediatric Health Med Ther [Internet]. 2019[citado em 2022 jan. 6];10:21-31. Disponível em: https://pubmed.ncbi.nlm.nih.gov/31040740/
Kakaroukas A, Abrahamse-Berkeveld M, Hayes L, McNally RJQ, Berrington JE, van Elburg RM, et al. Early infancy growth, body composition and type of feeding in late and moderate preterms. Pediatr Res [Internet] 2022[citado em 2023 maio 26]. Disponível em: https://doi.org/10.1038/s41390-022-02317-z
Fernandez JM, Ochoa, JJ, Dada GOL, Castro JD. Iron Deficiency and Iron Homeostasis in Low Birth Weight Preterm Infants: A Systematic Review. Nutrients [Internet]. 2019[citado em 2022 jan. 5];11(5):1090. Disponível em: https://doi.org/10.3390/nu11051090
Resch B, Wörner C, Ozdemir S, Hubner M, Puchas C, Urlesberger B. Respiratory Syncytial Virus Associated Hospitalizations in Infants of 33 to 42 Weeksʼ Gestation: Does Gestational Age Matter?. Klin Padiatr [Internet]. 2019[citado em 2022 jan. 6];231(04):206-11. Disponível em https://www.thieme-connect.com/products/ejournals/abstract/10.1055/a-0868-0004
Tompsen AMV. Adaptação e avaliação de um instrumento para medir qualidade de vida em crianças a partir de oito meses de idade até cinco anos [dissertação]. Porto Alegre (RS): Faculdade de Medicina da PUCRS; 2010.
Morais MB. Prevalência de distúrbios gastrointestinais funcionais em lactentes nascidos prematuros [dissertação]. São Paulo (SP): Universidade Federal de São Paulo; 2019.
Camilleri M, Park SY, Scarpato E, Statiano A. Exploring hypotheses and rationale for causes of infantile colic. Neurogastroenterol Motil [Internet] 2017[citado em 2022 jan. 6];29(2):e12943. Disponível em: https://doi.org/10.1111/nmo.12943
Mai T, Fatheree NY, Gleason W, Liu Y, Rhoads JC. Infantile Colic: New Insights into an Old Problem. Gastroenterol Clin North America [Internet]. 2018[citado em 2020 out. 24];47(4):829-44. Disponível em: https://doi.org/10.1016/j.gtc.2018.07.008
Nam SK, Park S, Lee J, Jun YH. Clinical Characteristics of Infantile Colic. Neonatal Med [Internet]. 2019[citado em 2022 jan. 4];26(1):34-40. Disponível em: https://doi.org/10.5385/nm.2019.26.1.34
Perceval C, Szajewska H, Indrio F, Weizman Z, Vandenplas Y. Prophylactic use of probiotics for gastrointestinal disorders in children. Lancet Child Adolesc Health [Internet]. 2019[citado em 2022 jan. 4];3(9):655-62. Disponível em: https://doi.org/10.1016/S2352-4642(19)30182-8
Araújo AC, Granja AC, Oliveira AS, Gandra AIS, Ribeiro ÉKT, Barbosa GFM, et al. Problemas na alimentação infantil e sua associação com a doença do refluxo. Rev Eletrônica Acervo Saúde [Internet]. 2021[citado em 2023 maio 26];13(6):e7492. Disponível em: https://doi.org/10.25248/reas.e7492.2021
Franco JM, Pinheiro APSG, Vieira SCF, Barreto IDC, Gurgel RQ, Cocco RR, et al. Accuracy of serum IgE concentrations and papule diameter in the diagnosis of cow's milk allergy. J. Pediatr [Internet]. 2018[citado em 2022 jan. 5];94(3):279-85. Disponível em: https://doi.org/10.1016/j.jped.2017.06.022
Monteiro GRSS, Tavares ANS, Pedrosa ZVRS. The early food introduction and the risk of allergies: A review of the literature. Enferm Glob [Internet]. 2019[citado em 2022 jan. 5];7(54):485-98. Disponível em: http://dx.doi.org/10.6018/eglobal.18.2.345231
Luskin K, Mortazavi D, Bai-Tong S, Bertrand K, Chambers C, Schulkers-Escalante K, et al. Allergen Content and Protease Activity in Milk Feeds from Mothers of Preterm Infants. Breastfeed Med [Internet]. 2022[citado em 2023 maio 26];17(11):947-57. Disponível em: 10.1089/bfm.2022.0115
Sousa CA, Galvão CCL, Barros MBA, Carandina L, Goldbaum M, Pereira JCR. Respiratory diseases and associated factors: populationbased study in São Paulo, 2008-2009. Rev Saúde Pública [Internet]. 2012[citado em 2022 jan. 5];46(1):16-25. Disponível em: https://doi.org/10.1590/S0034-89102011005000082
Alba JM, Rubio MTR, Corullón SC, Montaneret EA. Respiratory morbidity, atopy and asthma at school age in preterm infants aged 32–35 weeks. Rev Eur J Pediatric [Internet]. 2019[citado em 2022 jan. 5];178:973-82. Disponível em: https://doi.org/10.1007/s00431-019-03372-1
Mallick AK, Venkatnarayan K, Thapar RK, Tewari VV, Shaw SC. Morbidity Patterns of Late Preterm Babies Born Small for Gestation. Rev Indian J Pediatr [Internet]. 2019[citado em 2022 jan. 5];86:578-83. Disponível em: https://doi.org/10.1007/s12098-019-02925-4
Gupta P, Mital R, Kumar B, Yadav A, Jain M, Upadhyay A. Physical growth, morbidity profile and mortality among healthy late preterm neonates. Rev Indian Pediatrics [Internet]. 2017[citado em 2022 jan. 5];54:629-34. Disponível em: https://doi.org/10.1007/s13312-017-1123-1
Oliviera BL, Ribeiro LM, Parente PRA, Del Alamo GLE, Vieira GB, Falcão KS. Profile of at-risk newborns attended by nurses in outpatient follow-up clinic: a retrospective cohort study. Rev Latino-Am Enferm [Internet]. 2019[citado em 2022 jan. 5];27:e3113. Disponível em: https://doi.org/10.1590/1518-8345.2301.3113
Additional Files
Published
Issue
Section
License
Copyright (c) 2024 REME-Revista Mineira de Enfermagem

This work is licensed under a Creative Commons Attribution 4.0 International License.